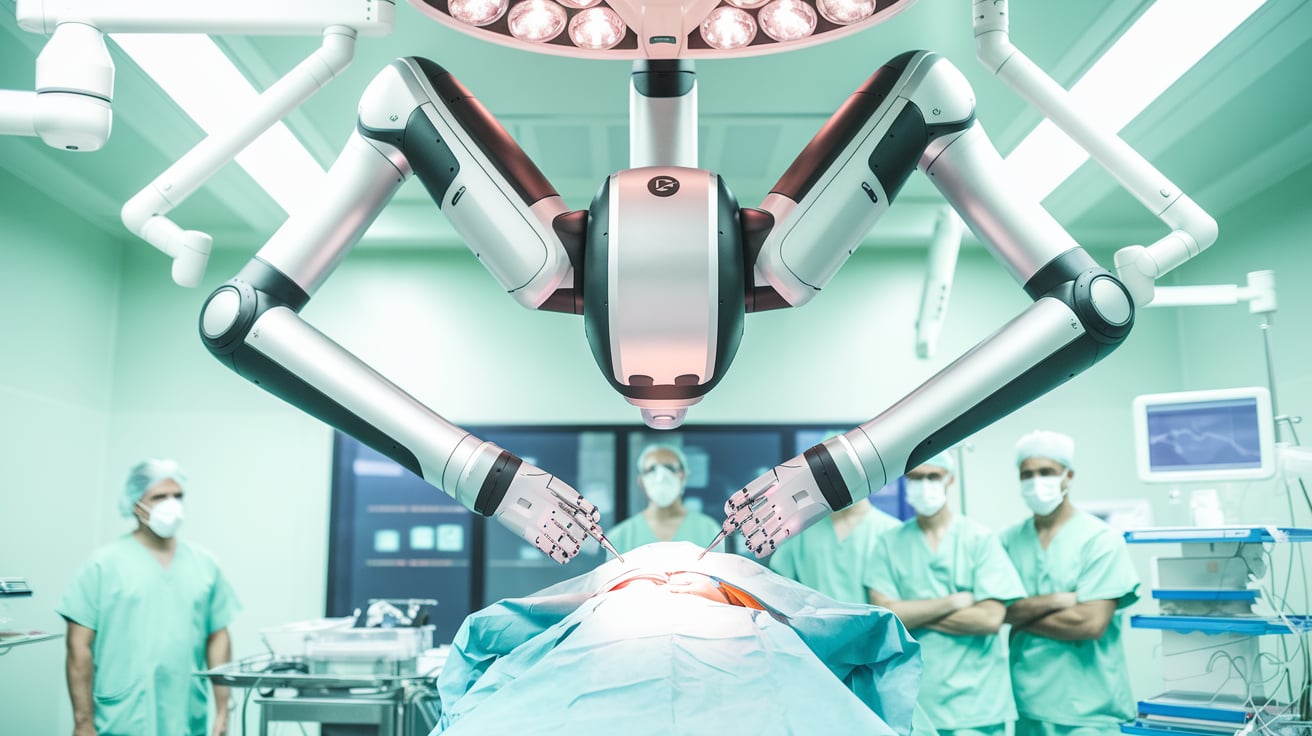
Mortality following transcatheter aortic valve replacement (TAVR), a procedure that has become a standard treatment for severe aortic stenosis, saw a decline in the years leading up to 2019 but began to rise again in 2020. A new study published in JACC: Cardiovascular Interventions reviews nearly 11 years of data to explore the reasons behind this troubling trend, which includes the potential influence of the COVID-19 pandemic and other underlying factors.
A Deep Dive into TAVR Mortality
From 2012 to 2018, the one-year mortality rate for TAVR patients decreased from 10.6% to 7.1%. However, by 2022, that rate had risen to 12.2%. The study’s authors, led by Dr. Dhaval Kolte of Massachusetts General Hospital, acknowledge the impact of the COVID-19 pandemic but suggest that several other factors may have contributed to the increase.
The Role of COVID-19
The authors speculate that the rise in mortality may be attributed to COVID-19, which caused delays in procedures and worsened overall health outcomes. Research has shown that TAVR patients who underwent procedures during COVID-19 surges had higher predicted risk scores, longer wait times for surgery, and poorer outcomes compared to those treated before or after pandemic waves. Additionally, CMS policy changes in 2019 and FDA approval for TAVR in low-risk patients may have led to more procedures being conducted at new centers, which often have lower volumes and thus higher mortality rates.
Noncardiac Deaths Are Common
Interestingly, noncardiac causes of death were responsible for nearly 69% of all deaths in the first year after TAVR. Pulmonary issues, infections, and neurological complications were the leading causes of these deaths. Patients with chronic lung disease, home oxygen use, and a history of atrial fibrillation were found to be particularly at risk.
Key Risk Factors for Increased Mortality
The study identified several risk factors associated with higher mortality after TAVR:
- Age over 80
- Chronic lung disease
- History of stroke or myocardial infarction
- Peripheral artery disease
- Nonfemoral access sites
- Non-elective procedures
Certain complications, including aortic dissection, cardiac arrest, and renal failure, were also linked to an increased risk of death. The authors emphasize that while some of these complications are unpredictable, a careful procedure and strong post-operative care can reduce risk.
Future Research Needed
Despite these findings, the study’s authors caution that further research is needed to fully understand the pandemic’s long-term impact on TAVR outcomes and to explore how changes in patient demographics, hospital volumes, and clinical practices may have affected mortality rates.
Follow MEDWIRE.AI for more updates on TAVR and cardiovascular health.